A ventilator machine is a life-support device that mechanically assists or replaces spontaneous breathing by delivering controlled volumes of oxygen-enriched air to patients’ lungs using positive pressure. These sophisticated medical devices monitor respiratory parameters, provide various ventilation modes, and include comprehensive safety systems to support patients with respiratory failure.
Picture this: You’re responding to a code blue at 2 AM, and the patient’s oxygen saturation is plummeting despite your best efforts with a bag-valve mask. Their diaphragm, weakened by pneumonia, simply can’t generate the pressure needed to inflate their lungs. This is the moment when decades of biomedical engineering innovation become the difference between life and death—when that sophisticated machine in the corner transforms from equipment to lifeline.
Whether you’re a student wondering how that complex device actually sustains breathing, a BMET troubleshooting alarms in the middle of the night, or a clinical engineer evaluating procurement options, understanding ventilator technology isn’t just academic knowledge. It’s the foundation that helps you make decisions that directly impact patient outcomes every single day.
Table of Contents
- Beyond the Basics: What Makes a Ventilator More Than an "Air Pump"
- The Engineering Marvel Behind Every Breath
- Ventilator Modes: Matching Technology to Patient Needs
- The Science Behind Each Breath
- Critical Settings That Make the Difference
- Safety Systems: Your First Line of Defense
- Common Ventilator Alarm Troubleshooting
- Real-World Applications: Where Ventilators Save Lives
- From Iron Lungs to AI: The Evolution Continues
- Liberation: The Art and Science of Weaning
- For Biomedical Professionals: Your Critical Role
Beyond the Basics: What Makes a Ventilator More Than an “Air Pump”
We’ve all heard ventilators described as “breathing machines” or “air pumps,” but that’s like calling a Formula 1 race car a “fancy bicycle.” A mechanical ventilator is a precision life-support system that doesn’t just move air—it orchestrates the entire process of respiration when patients can’t breathe adequately on their own.[1][2]
Here’s what’s really happening: While your healthy lungs use negative pressure (think of your diaphragm creating a vacuum that sucks air in), ventilators flip the script entirely. They use positive pressure ventilation—essentially pushing air directly into the lungs. It’s the difference between sipping through a straw and having someone gently inflate a balloon inside your chest.[3][4]
But here’s where it gets interesting: modern ventilators don’t just push air. They maintain precise positive end-expiratory pressure (PEEP) to prevent your alveoli from collapsing like deflated balloons, deliver exactly calibrated volumes based on your body weight and lung condition, and continuously monitor dozens of parameters to ensure optimal care. When you’re managing a patient on a ventilator, you’re not just providing air—you’re providing hope.[5]
Key Ventilator Terms Glossary
PEEP: Positive End-Expiratory Pressure – maintains lung inflation during expiration (typically 5-20 cmH₂O)
FiO₂: Fraction of Inspired Oxygen – percentage of oxygen in delivered air (21-100%)
I:E Ratio: Inspiratory-to-Expiratory time ratio – typically 1:2 or 1:3 for normal breathing
Tidal Volume: Amount of air delivered per breath (6-8 mL/kg ideal body weight)
SIMV: Synchronized Intermittent Mandatory Ventilation – combines mandatory and spontaneous breaths
PSV: Pressure Support Ventilation – assists patient-initiated breaths
Auto-PEEP: Inadvertent positive pressure from incomplete exhalation
Compliance: Lung elasticity measurement (normal: 50-100 mL/cmH₂O)
The Engineering Marvel Behind Every Breath
Understanding how ventilators work means looking at three interconnected systems working in perfect harmony—each one critical to maintaining life.[6][7]
The Power and Gas Foundation
Your ventilator needs two types of power to function: electrical for the brains and compressed gases for the muscle. Those medical air and oxygen lines delivering precisely 400 kPa aren’t just convenient—they’re your lifeline when the main power fails. The redundancy built into these systems reflects something every biomedical professional knows: when equipment fails, patients suffer.[6]
The gas blending system is where precision engineering really shines. Modern turbine-driven ventilators can adjust oxygen concentration from room air (21%) to pure oxygen (100%) with the turn of a dial. This isn’t just convenience—it’s the difference between providing just enough oxygen and risking toxicity from too much.[8][6]
The Intelligent Control System
Here’s where modern ventilators separate themselves from their predecessors: microprocessor-controlled systems that think ahead. Closed-loop systems don’t just deliver what you set—they continuously measure what the patient actually receives and adjust accordingly.[7]
Think of it this way: older open-loop systems are like pouring coffee without looking at the cup size. They deliver exactly what you program, regardless of whether the patient’s lungs can handle it. Modern closed-loop systems are like having an experienced barista who adjusts the pour based on your mug—they monitor patient compliance, airway resistance, and delivered volumes, then make real-time adjustments to optimize care.[7]
This intelligence enables features like adaptive pressure support and automated weaning protocols that don’t just reduce your workload—they often deliver better patient outcomes than manual adjustments alone.
The Patient Interface: More Than Tubing
Those circuits connecting ventilator to patient represent sophisticated engineering designed for safety. Compliance compensation accounts for the volume lost as tubing expands under pressure—typically 1-3 mL per cmH₂O, which might not sound like much until you realize that’s 20-60 mL of every breath that never reaches the patient without compensation.[7]
The integrated humidification systems aren’t just comfort features—they’re preventing the airway damage that occurs when dry, cold gases irritate delicate lung tissues. And those pressure release valves? They’re your fail-safe against the lung injury that can occur when pressures exceed safe limits.[9]
Ventilator Modes: Matching Technology to Patient Needs
When you’re standing at a ventilator adjusting settings, you’re not just turning dials—you’re choosing from sophisticated strategies developed over decades of clinical research. Each mode represents a different philosophy of how to best support breathing.[10]
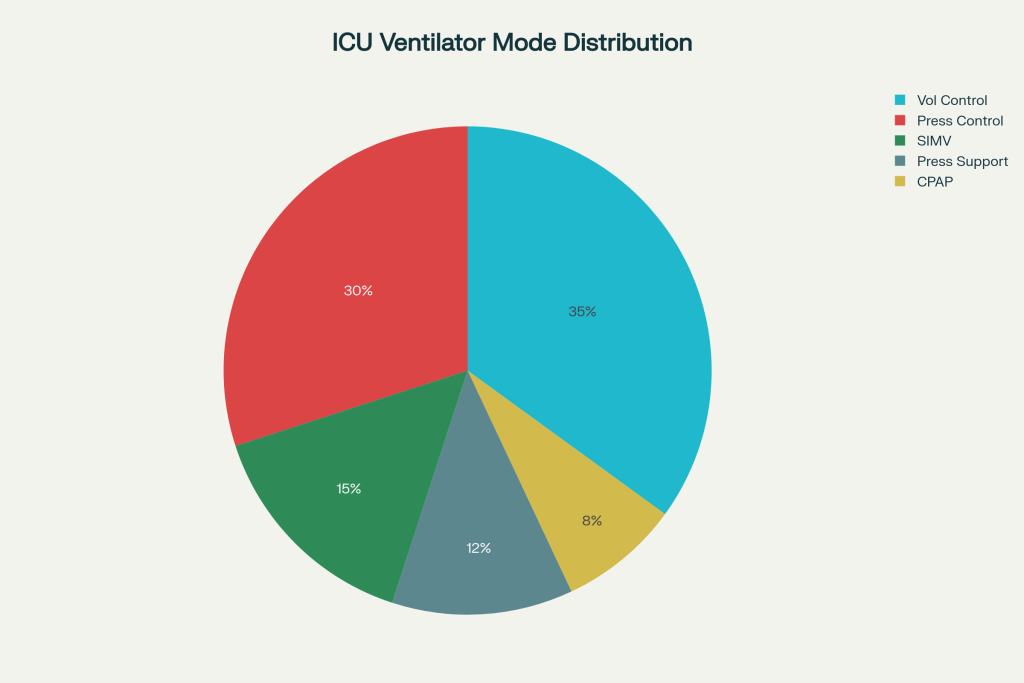
Ventilator Modes Comparison
| Mode | Delivery Method | Best Applications | Key Advantage | Main Limitation | Typical Settings |
| Volume Control (VCV) | Fixed tidal volume (6-8 mL/kg) | Anesthesia, stable lung mechanics | Predictable minute ventilation | High pressure risk with poor compliance | TV: 400-500mL, RR: 12-20 |
| Pressure Control (PCV) | Fixed pressure limit (15-30 cmH₂O) | ARDS, lung protection strategies | Prevents barotrauma | Variable tidal volume requires monitoring | PC: 20-25 cmH₂O, RR: 16-24 |
| SIMV | Mandatory + spontaneous breaths | Weaning from mechanical ventilation | Gradual transition to independence | Complex monitoring requirements | Rate: 6-12, PS: 8-15 cmH₂O |
| Pressure Support (PSV) | Patient-triggered pressure boost | Alert patients, spontaneous breathing | Comfortable, responsive breathing | Requires active patient participation | PS: 10-20 cmH₂O |
| CPAP | Continuous positive pressure | Sleep apnea, mild respiratory support | Non-invasive, maintains recruitment | Limited to hemodynamically stable patients | CPAP: 5-15 cmH₂O |
Volume Control Ventilation: Predictable but Unforgiving
In Volume Control (VCV) mode, the ventilator delivers exactly the tidal volume you set—typically 6-8 mL per kilogram of ideal body weight. This predictability is crucial when you need consistent minute ventilation, like during anesthesia or for neurologically impaired patients with stable lung mechanics.[8][11]
But here’s the challenge you face: if the patient’s lungs become stiffer (think ARDS or pneumonia), pressures can skyrocket to dangerous levels. You’re constantly balancing the need for adequate ventilation against the risk of ventilator-induced lung injury—a reminder that every setting matters.
Pressure Control: Lung Protection with Trade-offs
Pressure Control (PCV) mode flips the priority: it delivers breaths to your preset pressure limit, letting tidal volume vary based on lung compliance. When you’re managing ARDS patients or anyone requiring lung-protective strategies, this mode becomes your ally in preventing barotrauma.[5][11]
The trade-off? Variable minute ventilation means you’re monitoring more closely, adjusting more frequently. But for patients whose lungs are fragile, that extra attention often pays dividends in outcomes.
SIMV and PSV: Supporting the Journey to Independence
Synchronized Intermittent Mandatory Ventilation (SIMV) and Pressure Support Ventilation (PSV) represent the bridge between full support and independence. When you’re weaning a patient, these modes let them take increasing responsibility for their breathing while providing a safety net.[10][12]
SIMV provides backup mandatory breaths while allowing spontaneous efforts between them. PSV boosts every patient-initiated breath, helping overcome the work of breathing through artificial airways. Both require an engaged, recovering patient—and both remind us that the goal isn’t just sustaining life, but returning it to the patient’s control.
The Science Behind Each Breath
Every respiratory cycle your ventilator delivers follows four precisely orchestrated phases. Understanding this cycle helps you troubleshoot problems, optimize settings, and explain what’s happening to families asking tough questions.[13]
Triggering: The Decision to Breathe
The cycle begins when your ventilator detects either a time interval (controlled modes) or patient effort (assisted modes). Those trigger sensitivity settings—typically -2 cmH₂O pressure or 2 L/min flow deviation—represent a delicate balance.[8][13]
Set sensitivity too high, and weak patients can’t trigger breaths, leading to respiratory muscle fatigue and patient-ventilator dyssynchrony. Set it too low, and the ventilator may auto-cycle, delivering unnecessary breaths that can cause discomfort and hemodynamic compromise. Getting this right often means the difference between a comfortable patient and one fighting the machine.[14]
Inspiration: Delivering Life-Sustaining Gas
During inspiration, your ventilator delivers the prescribed gas mixture according to your selected mode. Those settings you adjust—tidal volume, inspiratory flow rate, FiO₂—directly influence patient outcomes:[13]
- Tidal Volume: Those 350-550 mL for average adults represent more than numbers. They’re calculated based on ideal body weight because lung size correlates with height, not actual weight[11]
- Flow Rate: Typically 60 L/min but adjustable up to 120 L/min for patients with airflow obstruction who need their inspiratory time shortened[8]
- FiO₂: From 21% to 100%, titrated to maintain adequate oxygenation while minimizing oxygen toxicity risk[8]
The Transition: Knowing When to Stop
Cycling from inspiration to expiration happens based on your mode settings: time in volume control, pressure achievement in pressure control, or flow decay in pressure support. This timing affects everything from patient comfort to air trapping risk.[13]
Expiration: The Often-Overlooked Phase
Expiration typically occurs passively through elastic recoil, but PEEP changes everything. Those 5-20 cmH₂O of positive end-expiratory pressure prevent alveolar collapse and improve oxygenation.[5][13][15]
When you set PEEP, you’re applying one of mechanical ventilation’s most important advances. Those positive pressures keep recruitment channels open, preventing the repetitive opening and closing of alveoli that can cause ventilator-induced lung injury. It’s not just a setting—it’s lung protection in action.[15][16]
Critical Settings That Make the Difference
Every parameter you adjust on a ventilator carries clinical significance. Understanding how these settings interact helps you optimize patient care while avoiding common pitfalls.[8][11]
PEEP: The Unsung Hero of Mechanical Ventilation
When you apply PEEP, you’re preventing one of the most common complications of mechanical ventilation: atelectasis. Standard PEEP of 5 cmH₂O benefits most patients by counteracting the effects of intubation, sedation, and supine positioning.[5][8][15]
Higher PEEP levels (8-20 cmH₂O) become crucial for ARDS patients, often allowing you to reduce FiO₂ requirements and minimize oxygen toxicity risk. But here’s what you need to watch: excessive PEEP can impede venous return in volume-depleted patients or overdistend healthy lung regions while failing to recruit diseased areas. Every patient requires individual titration.[8][5]
Tidal Volume: The Paradigm Shift
Here’s something that changed everything we thought we knew about mechanical ventilation: large tidal volumes kill patients. The discovery that traditional 10-12 mL/kg volumes increased mortality in ARDS patients led to the lung-protective ventilation strategy using 6-8 mL/kg ideal body weight.[8][16]
This represents more than a setting change—it’s a fundamental shift from maintaining “normal” physiology to accepting permissive hypercapnia in favor of preventing mechanical lung injury. When you set lower tidal volumes, you’re applying evidence that directly saves lives.
Respiratory Rate and I:E Ratios: The Balancing Act
Respiratory rates of 12-20 breaths per minute must balance with tidal volume to achieve adequate minute ventilation. But the inspiratory-to-expiratory (I:E) ratio often matters more than the rate itself.[8][11]
Normal 1:2 or 1:3 ratios allow adequate expiratory time, but patients with COPD or asthma often need 1:4 or longer to prevent air trapping and auto-PEEP. When you hear about patient-ventilator dyssynchrony, inadequate expiratory time is often the culprit.[8]
Safety Systems: Your First Line of Defense
Modern ventilators incorporate comprehensive alarm systems designed to alert you to potentially life-threatening situations. Understanding these alarms isn’t just about stopping the noise—it’s about rapid problem recognition and resolution.[9][14][17]
High-Priority Alarms: When Seconds Count
Apnea alarms activate within 20 seconds of the last detected breath. This alarm most commonly indicates circuit disconnection—an immediately life-threatening situation requiring instant manual ventilation until you resolve the problem. Every biomedical professional should know this alarm by sound.[14]
High-pressure alarms warn of excessive airway pressures that could cause pneumothorax or other lung injury. Common causes include secretions, patient coughing, kinked tubes, or worsening compliance. Your response needs to be systematic: assess the patient first, then troubleshoot the circuit.[9][14]
Low-pressure alarms typically indicate leaks—circuit connections, cuff deflation, or disconnection. These compromise ventilation effectiveness and require immediate assessment and correction.[14]
Understanding Medium-Priority Alarms
PEEP alarms indicate deviations from your prescribed levels. High PEEP warnings may suggest auto-PEEP from inadequate expiratory time, while low PEEP alarms often indicate circuit leaks or equipment malfunction.[14]
Power failure alarms activate during electrical disruptions, automatically switching to battery backup while alerting you to the limited duration of emergency power. Most hospital-grade ventilators provide 30-60 minutes of battery operation—enough time for generator activation or patient transport.[9]
Common Ventilator Alarm Troubleshooting
When alarms sound at 3 AM, systematic troubleshooting saves lives. Here’s your step-by-step approach for the most common ventilator alarms:
High Pressure Alarm (Most Common: >40 cmH₂O)
Immediate Actions:
- Assess the patient first – Look for coughing, agitation, or distress
- Check airway – Secretions, biting endotracheal tube, bronchospasm
- Inspect circuit – Kinks in tubing, water accumulation in lines
- Evaluate lung compliance – Listen for pneumothorax, assess chest rise
Common Causes & Solutions:
- Secretions: Suction airway, consider mucolytics
- Patient coughing: Check sedation, ensure synchrony
- Kinked tubing: Straighten circuit, secure connections
- Pneumothorax: Immediate chest decompression may be needed
Low Pressure Alarm (Most Critical)
Immediate Actions:
- Look for obvious disconnection – Most common cause
- Manual ventilation – Use bag-valve mask immediately if needed
- Check endotracheal tube cuff – May be deflated
- Inspect all connections – Ventilator to circuit to patient
Common Causes & Solutions:
- Circuit disconnection: Reconnect immediately, check all fittings
- Cuff leak: Re-inflate cuff, check for tube migration
- Ventilator malfunction: Switch to backup ventilator if available
Apnea Alarm
Immediate Actions:
- Assess patient responsiveness – Check for spontaneous breathing
- Verify trigger sensitivity – May be set too low for weak patients
- Check circuit for leaks – Small leaks prevent trigger detection
- Manual ventilation – If patient truly apneic
PEEP Deviation Alarms
High PEEP (Auto-PEEP):
- Increase expiratory time (lower I:E ratio)
- Check for airway obstruction
- Reduce respiratory rate if possible
- Consider bronchodilators for obstructive disease
Low PEEP:
- Check circuit for leaks
- Verify PEEP valve function
- Inspect expiratory valve operation
Power/Battery Alarms
Immediate Actions:
- Verify main power connection – Check power cord and outlet
- Assess battery level – Most provide 30-60 minutes backup
- Prepare for transport – If extended outage expected
- Manual ventilation backup – Always have bag-valve mask ready
💡 Pro Tip for BMETs: Keep a laminated troubleshooting card with your most critical patients. When alarms sound, systematic approach beats panic every time. Document resolution steps for quality improvement and staff training.
Real-World Applications: Where Ventilators Save Lives
Ventilators serve diverse roles throughout healthcare, each requiring specific capabilities and expertise. Understanding these applications helps you make informed decisions about equipment selection and management.[2][18]
ICU Ventilation: The Front Lines
ICU ventilators support the sickest patients with complex pathophysiology requiring multiple modes, advanced monitoring, and integration with other life-support technologies. These patients often remain on ventilation for days to weeks, requiring equipment capable of long-term operation with minimal maintenance.[18][19][20]
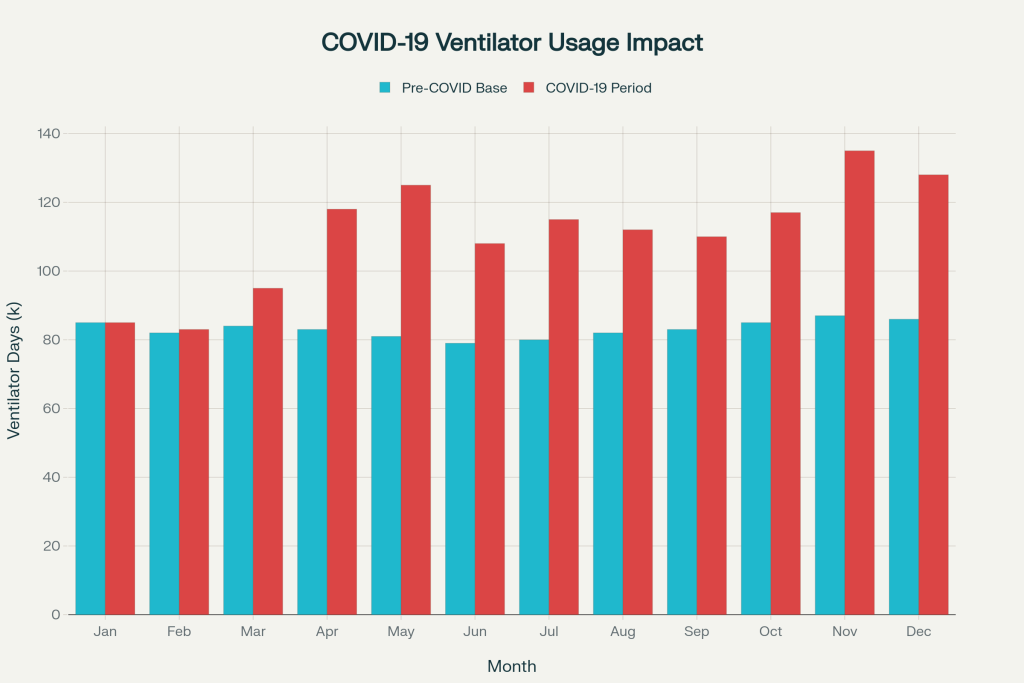
Monthly mechanical ventilator usage in the United States during 2020, showing the dramatic 38% increase during the COVID-19 pandemic compared to pre-pandemic baseline levels.
Recent analysis shows that mechanical ventilator utilization has stabilized at approximately 15% above pre-pandemic levels as of 2025, reflecting both increased ICU capacity and improved non-invasive ventilation strategies. This sustained demand highlights the critical importance of adequate ventilator capacity and the specialized expertise required to operate these sophisticated devices effectively.
Transport and Emergency: Mobility Under Pressure
Transport ventilators must provide reliable ventilation in challenging environments with limited power and extreme portability requirements. These devices support patients during ambulance transport, emergency department resuscitation, and interfacility transfers.[21]
The unique challenges—vibration resistance, battery longevity, operation across varying altitudes—require engineering solutions that prioritize reliability over features. When you’re managing a critically ill patient in an ambulance, equipment failure isn’t just inconvenient—it’s catastrophic.
Home Ventilation: Technology Enabling Life
The growing population requiring long-term mechanical ventilation has driven development of sophisticated home ventilators supporting patients with ALS, high spinal cord injuries, and severe COPD. These devices allow patients to live outside institutional settings while receiving necessary respiratory support.[22]
Home ventilators require exceptional reliability since professional technical support may not be immediately available. They must operate quietly to avoid disturbing household routines and provide clear alarm systems for family caregivers who may not have medical training.
Current trends show a 40% increase in home ventilator utilization since 2020, driven by improved technology, better insurance coverage, and patient preference for home-based care when medically appropriate.
From Iron Lungs to AI: The Evolution Continues
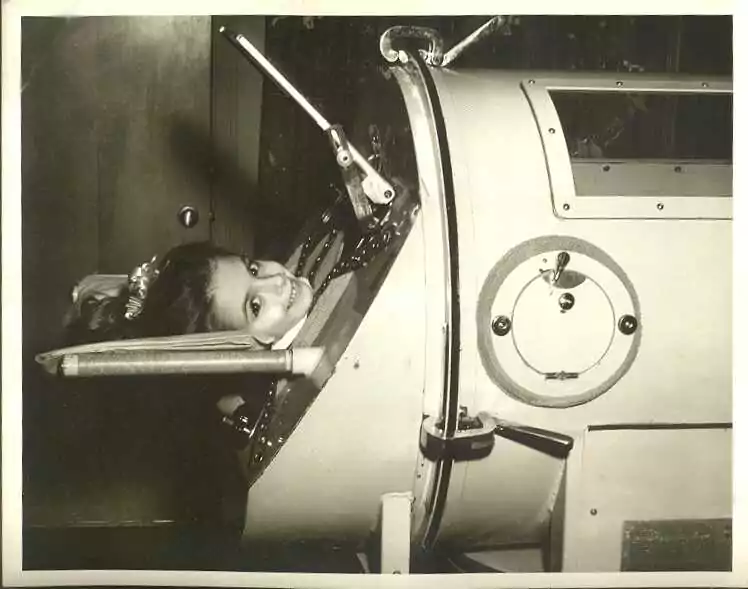
Historic iron lung ventilator illustrating negative pressure assisted breathing in polio treatment.
Understanding where ventilator technology came from helps appreciate where it’s heading. The iron lung, developed at Harvard in 1928, weighed up to 650 pounds and completely encased patients in an airtight cylinder. During polio epidemics, these devices filled hospital wards, supporting thousands with respiratory paralysis.[23][24][25][26]
The transition to positive pressure ventilation in the 1950s enabled modern ICU medicine. Today’s ventilators incorporate microprocessor control, sophisticated monitoring, and adaptive algorithms that automatically adjust to patient needs.[26][27][28]
Current Innovations in Ventilator Technology
Artificial Intelligence Integration: Modern ventilators incorporate machine learning algorithms that predict patient needs, automatically adjust settings, and provide early warning of clinical deterioration. AI-driven parameter optimization reduces clinician workload while improving patient synchrony.
Smart Connectivity: Cloud-based monitoring systems enable remote oversight, predictive maintenance alerts, and real-time performance analytics across hospital networks. This connectivity proved crucial during COVID-19 for managing surge capacity.
Patient-Synchronized Technology: Advanced flow sensors and pressure monitoring create more comfortable, responsive ventilation that adapts to patient breathing patterns in real-time, reducing the need for sedation and accelerating weaning.
Liberation: The Art and Science of Weaning
Perhaps the most critical aspect of mechanical ventilation involves safely discontinuing support when patients recover sufficient respiratory function. Ventilator weaning represents both art and science, requiring careful assessment and gradual support reduction.[20][29][30]
Readiness: More Than Just Numbers
Before initiating weaning trials, patients must demonstrate stability across multiple systems. Key criteria include adequate oxygenation on modest support (FiO₂ < 50%, PEEP ≤ 8 cmH₂O), hemodynamic stability, and sufficient respiratory muscle strength.[12][20]
But here’s what experience teaches: successful weaning depends on more than meeting criteria. Adequate nutrition supports respiratory muscle strength, early mobility prevents ICU-acquired weakness, and minimizing sedation allows accurate assessment of respiratory drive.[20][12]
The Spontaneous Breathing Trial: The Gold Standard
Spontaneous breathing trials (SBTs) lasting 30-120 minutes remain the best predictor of extubation success. During trials, patients breathe through minimal support while you monitor for respiratory distress signs.[29]
Protocol-driven weaning approaches consistently reduce ventilator duration compared to individualized physician-directed weaning. This isn’t about replacing clinical judgment—it’s about applying evidence-based practices that improve outcomes.[12]
Weaning Protocol Checklist
Daily Readiness Assessment:
✅ FiO₂ ≤ 50% with adequate oxygenation
✅ PEEP ≤ 8 cmH₂O maintaining oxygen saturation >90%
✅ Hemodynamically stable (no significant vasopressors)
✅ Afebrile (<38.5°C) without active infection
✅ Adequate mental status for airway protection
✅ Minimal sedation requirements
SBT Parameters:
- Duration: 30-120 minutes
- Support: T-piece, PSV 5-8 cmH₂O, or CPAP 5 cmH₂O
- Monitor: Respiratory rate, tidal volume, oxygen saturation
- Success criteria: RR <35, no accessory muscle use, adequate gas exchange
For Biomedical Professionals: Your Critical Role
As biomedical engineers and technicians, ventilators represent some of your most complex and critical equipment. Your understanding of operation, maintenance requirements, and clinical applications directly impacts patient safety and outcomes.[6][31]
Procurement: Looking Beyond Specifications
When evaluating ventilator purchases, consider both immediate needs and future expansion capabilities. ICU ventilators should provide multiple modes, comprehensive monitoring, and advanced alarm systems for complex patients. Transport ventilators prioritize portability and battery life, while home ventilators emphasize reliability and user-friendly interfaces.[10][22][32]
Your recommendations influence not just budgets but patient care capabilities. That decision to invest in advanced monitoring or additional safety features could prevent the complications that occur when equipment limitations meet clinical complexity.
Procurement Evaluation Framework:
- Clinical Capability: Modes available, monitoring parameters, alarm systems
- Integration: Compatibility with existing hospital systems and networks
- Reliability: MTBF ratings, service history, manufacturer support
- Total Cost of Ownership: Purchase price, maintenance contracts, staff training
- Future-Proofing: Software upgrade capability, emerging technology adoption
Maintenance: When Lives Depend on Reliability
Regular preventive maintenance ensures optimal performance when patients depend on these devices for survival. This includes calibrating sensors, replacing filters, testing alarms, and verifying battery backup functionality.[9][14]
But maintenance goes beyond scheduled tasks. It means understanding common failure modes, recognizing early warning signs, and having rapid response procedures for emergencies. When ventilator alarms sound at 3 AM, your expertise makes the difference between quick resolution and prolonged patient risk.
Essential Monthly Maintenance Tasks:
- Flow and pressure sensor calibration verification
- Battery backup capacity testing (should maintain 30+ minutes)
- Alarm system functionality check (all priority levels)
- Circuit leak testing and connection verification
- Software updates and security patches
- Environmental condition monitoring (temperature, humidity)
Training: Bridging Technology and Care
Ventilator complexity requires ongoing education for clinical staff. Your role often includes supporting training programs covering alarm management, basic troubleshooting, and emergency procedures.[17]
Understanding common alarm causes and appropriate responses enables rapid problem resolution while maintaining patient safety. When you help nursing staff recognize the difference between nuisance alarms and life-threatening alerts, you’re directly contributing to better patient outcomes.
Frequently Asked Questions
Q: What is a ventilator machine used for?
A: A ventilator machine supports or takes over the breathing process when patients cannot breathe effectively on their own due to illness, injury, or surgery. It delivers controlled amounts of oxygen-enriched air to the lungs while removing carbon dioxide, maintaining adequate gas exchange to sustain life.
Q: What are the most common ventilator modes?
A: The most common ventilator modes include Volume Control Ventilation (VCV) for predictable tidal volume delivery, Pressure Control Ventilation (PCV) for lung protection, Synchronized Intermittent Mandatory Ventilation (SIMV) for weaning, and Pressure Support Ventilation (PSV) for patient comfort during spontaneous breathing.
Q: What’s the main difference between a ventilator and a BiPAP machine?
A: A ventilator can fully take over or assist breathing, often through a tube in the airway, while a BiPAP delivers non-invasive support via a mask and helps with breathing but doesn’t replace it completely. check our comprehensive guide on Ventilator vs BiPAP.
Q: How do ventilators prevent lung injury?
A: Modern ventilators prevent lung injury through protective settings including low tidal volumes (6-8 mL/kg ideal body weight), appropriate PEEP levels to prevent alveolar collapse, pressure-limited modes to avoid barotrauma, and sophisticated monitoring to detect patient-ventilator dyssynchrony.
Q: What are the key safety features in modern ventilators?
A: Essential safety features include high and low pressure alarms, apnea detection with backup ventilation, power failure alerts with battery backup, PEEP monitoring, oxygen concentration verification, and comprehensive alarm systems with both audible and visual alerts to ensure immediate notification of critical situations.
Q: How is ventilator performance monitored?
A: Ventilator performance is monitored through continuous measurement of airway pressures, delivered and returned tidal volumes, respiratory rate and rhythm, oxygen saturation, end-tidal CO₂, patient-ventilator synchrony assessment, and trend analysis of all respiratory parameters over time.
Q: What’s the difference between invasive and non-invasive ventilation?
A: Invasive ventilation requires an endotracheal tube or tracheostomy to deliver positive pressure directly to the lungs, while non-invasive ventilation uses masks or nasal interfaces. Invasive ventilation provides more precise control and is used for critically ill patients, while non-invasive methods are preferred for less severe respiratory failure and patient comfort.
Q: How long can patients safely remain on mechanical ventilation?
A: Duration varies significantly based on underlying condition and patient factors. Short-term ventilation (hours to days) is common for surgery and acute illness recovery. Long-term ventilation (weeks to months) may be necessary for chronic conditions, with careful attention to preventing complications like ventilator-associated pneumonia and muscle weakness.
Q: What training do biomedical technicians need for ventilator maintenance?
A: BMETs should complete manufacturer-specific training on each ventilator model, understand respiratory physiology basics, master alarm troubleshooting procedures, learn preventive maintenance protocols, and maintain current knowledge of safety standards and regulatory requirements. Professional certification in biomedical engineering enhances credibility and expertise.
The Human Side of Technology
Mechanical ventilators represent one of medicine’s most sophisticated life-sustaining technologies, supporting millions of patients annually through respiratory failure, surgical procedures, and recovery. From iron lungs to today’s microprocessor-controlled devices, ventilators exemplify how biomedical innovation directly saves lives.[33]
Your expertise with ventilator technology—whether calibrating sensors, training staff, or evaluating new equipment—connects directly to someone’s ability to breathe. The lessons learned during the COVID-19 pandemic reminded us all of ventilators’ critical importance and the specialized knowledge required to operate them effectively.[34]
Every breath supported by mechanical ventilation represents a victory of human ingenuity over respiratory failure. Understanding how these remarkable machines work, and keeping them working when it matters most, remains one of the most important contributions you make to modern healthcare.
When equipment fails, you respond. When alarms sound, you troubleshoot. When new technology emerges, you evaluate and implement it. Behind every successful ventilator intervention stands a biomedical professional who understood that technology and compassion aren’t opposites—they’re partners in the mission to preserve and restore life.
That understanding, that expertise, that dedication to getting it right when seconds count—that’s what makes you more than just a technician or engineer. That’s what makes you an essential part of the healthcare team, ensuring that when patients can’t breathe on their own, the technology that sustains them works flawlessly, every single time.
Have questions about ventilator technology or want to share your experience? Join the discussion in our biomedical engineering community forum where professionals collaborate and learn from each other’s expertise.
- https://en.wikipedia.org/wiki/Ventilator
- https://www.healthline.com/health/ventilator
- https://www.uab.edu/news/health-medicine/how-a-ventilator-works-and-why-you-don-t-want-to-need-one
- https://emedicine.medscape.com/article/304068-overview
- https://my.clevelandclinic.org/health/treatments/15368-mechanical-ventilation
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8080500/
- https://ecampusontario.pressbooks.pub/mcvresource/chapter/2-1-ventilators-the-basics/
- https://www.msdmanuals.com/professional/critical-care-medicine/respiratory-failure-and-mechanical-ventilation/overview-of-mechanical-ventilation
- https://derangedphysiology.com/main/cicm-primary-exam/respiratory-system/Chapter-511/alarms-and-safety-features-mechanical-ventilation
- https://www.prepladder.com/neet-pg-study-material/dermatology-and-venereology/modes-of-ventilation-types-and-uses
- https://www.youtube.com/watch?v=gnfCg3RXtGk
- https://elsevier.health/en-US/preview/mechanical-vent-weaning
- https://www.ncbi.nlm.nih.gov/books/NBK539742/
- https://www.respiratorytherapyzone.com/ventilator-alarms/
- https://www.criticalcarepractitioner.co.uk/mechanical-ventilation-peep-positive-end-expiratory-pressure/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7428118/
- https://tracheostomyeducation.com/mechanical-ventilator-alarms/
- https://www.medanta.org/patient-education-blog/the-life-saving-role-of-ventilators-in-icu
- https://www.apexhospitals.com/procedure/mechanical-ventilation
- https://litfl.com/weaning-from-mechanical-ventilation/
- https://sisurgical.co.in/blog/the-role-of-icu-ventilators-in-emergency-medical-care
- https://www.bajajfinserv.in/ventilator-machine
- https://pubmed.ncbi.nlm.nih.gov/2205164/
- https://en.wikipedia.org/wiki/Iron_lung
- https://www.sciencemuseum.org.uk/objects-and-stories/medicine/iron-lung
- https://www.bbc.com/future/article/20240315-iron-lung-led-to-creation-of-modern-day-intensive-care-unit
- https://pubmed.ncbi.nlm.nih.gov/32809751/
- https://www.linkedin.com/pulse/innovations-ventilator-technology-biome-healthcare-private-limited-fxnfc
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4893753/
- https://www.ncbi.nlm.nih.gov/books/NBK430712/
- https://knowhow.distrelec.com/medical-healthcare/medical-ventilators-a-breakdown-of-the-components-and-sensors-needed-in-essential-medical-care/
- https://www.youtube.com/watch?v=yDtKBXOEsoM
- https://www.aast.org/resources-detail/mechanical-ventilation-in-intensive-care-unit
- https://pmc.cbi.nlm.nih.gov/articles/PMC9993519