It’s 2:47 AM in the cardiac ICU when the ECG machine starts throwing error codes you’ve never seen. The patient in bed 3 is showing concerning symptoms, but your primary diagnostic tool just went dark.
Sound familiar? If you’re a biomedical engineer, ECG technician, or healthcare professional responsible for cardiac monitoring equipment, you’ve probably been in this exact situation, where theoretical knowledge meets the harsh reality of equipment failure when lives are on the line.

This isn’t another basic overview of ECG machines. Instead, we’re diving into what really matters: how these critical devices actually work in practice, why they fail, and what you can do about it when they do.
Because understanding your ECG machine isn’t just technical knowledge, it’s patient care.
The Hidden Reality: Why ECG Knowledge Matters More Than Ever
Before we explore the technical details, let’s acknowledge something most textbooks won’t tell you: ECG equipment downtime costs hospitals an average of $12,000+ per hour in delayed procedures.
More importantly, research shows that up to 64% of ECG leads are misplaced during routine procedures, leading to 17-24% of cases requiring diagnostic reinterpretation.
These aren’t just statistics; they represent real patients whose care depends on your equipment working flawlessly and your team understanding how to use it correctly.
What Really Happens Inside an ECG Machine
The Signal Journey: From Heartbeat to Display
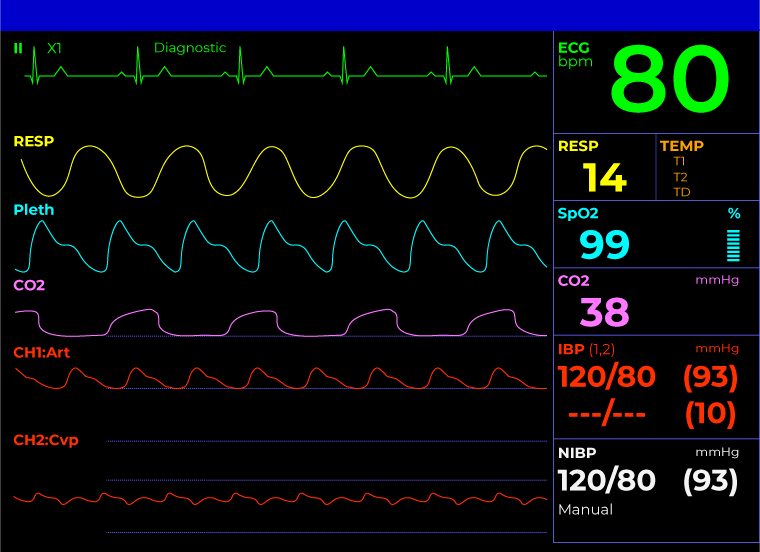
An ECG machine performs what seems like magic: it captures electrical signals from the heart that are smaller than radio static and transforms them into the clear waveforms you see on screen.
Here’s what actually happens during those critical first milliseconds:

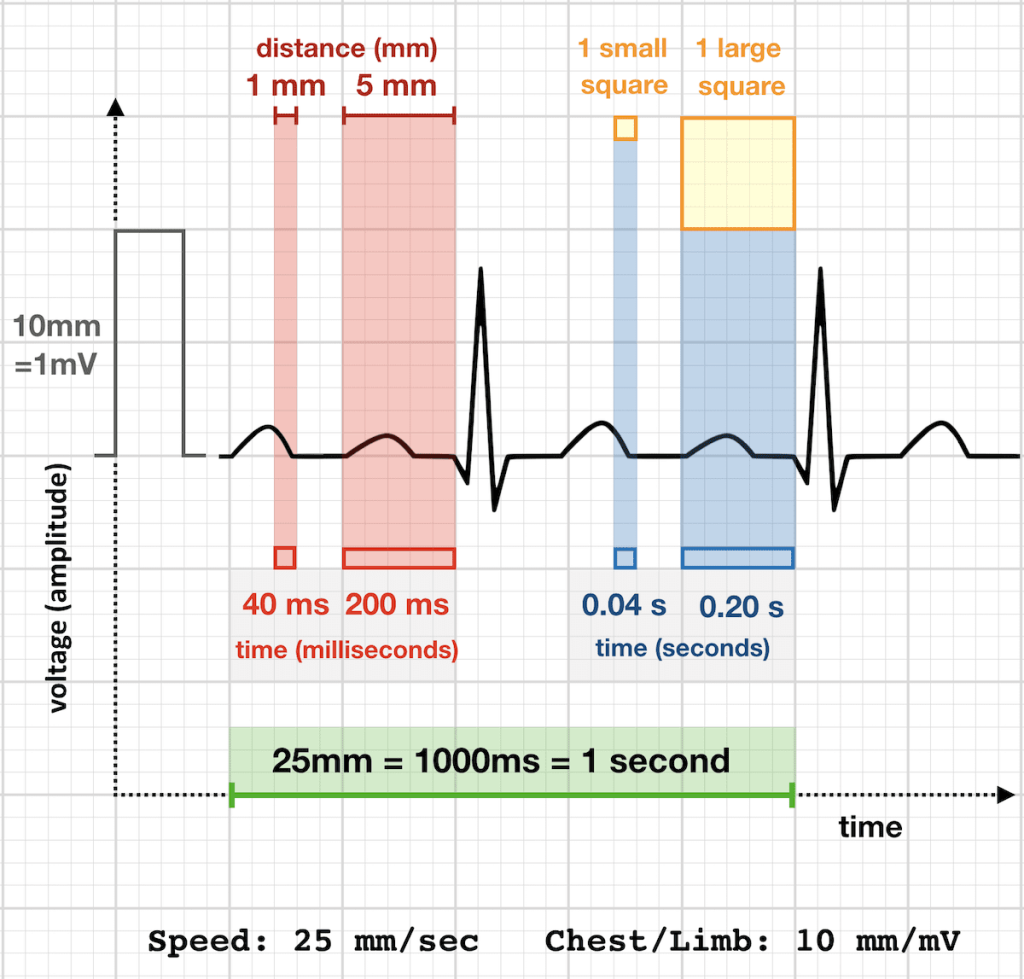
Signal Acquisition: The heart generates electrical impulses measuring just 1-2 millivolts, that is 1/1000th of the voltage in a standard battery. Your ECG machine must detect these tiny signals while filtering out electrical noise from fluorescent lights, cell phones, and the dozen other electronic devices in every modern hospital room.
Amplification: The machine amplifies these signals by a factor of 1,000 or more. This is where many problems start; if your amplification circuits drift even slightly, you’ll see baseline wander, signal distortion, or complete signal loss. This is why proper calibration isn’t just recommended, it’s essential for accurate diagnosis.
Digital Conversion: Modern ECG machines convert analog heart signals into digital data at rates of 500-1000 samples per second. This digital conversion allows for computer analysis, storage, and transmission, but it also introduces potential points of failure that earlier analog machines didn’t have.
The 13 Essential Components: Beyond Basic Descriptions
Most resources mention 7 basic ECG components, but real-world operation involves 13 critical elements that can affect your machine’s performance:

Standard Components:
- Electrodes and lead wires
- Amplification circuits
- Display system
- Recording/printing mechanism
- Power supply and battery backup
Often Overlooked Components:
- Isolation circuits: Protect patients from electrical shock and eliminate ground loops
- Right-leg driver circuit: Reduces common-mode noise by up to 90dB
- Calibration signal generator: Produces the standard 1mV square wave for testing
- Digital filtering systems: Remove baseline drift and high-frequency noise
- Patient safety circuits: Monitor for lead-off conditions and electrical faults
- Data processing unit: Handles signal analysis and automatic interpretation
- Communication interfaces: Enable connectivity with EMR systems and networks
- Environmental sensors: Monitor temperature and humidity that affect signal quality
Understanding these additional components helps explain why ECG machines fail and how to troubleshoot them effectively.
How ECG Machines Work: The Practical Operation
Signal Processing: The Technical Reality
When a patient’s heart contracts, it creates a moving wave of electrical depolarization. ECG electrodes act as antennas, picking up this electrical activity from different angles around the heart.
Here’s where it gets technically interesting:
The machine must simultaneously:
- Reject common-mode signals (electrical noise affecting all leads equally) while amplifying differential signals (the actual heart activity)
- Maintain input impedance above 10 megohms to avoid signal loading
- Filter frequencies outside the diagnostic range (typically 0.05-100 Hz for diagnostic ECGs)
- Compensate for electrode impedance variations that can cause signal artifacts.
The Lead System: More Complex Than It Appears
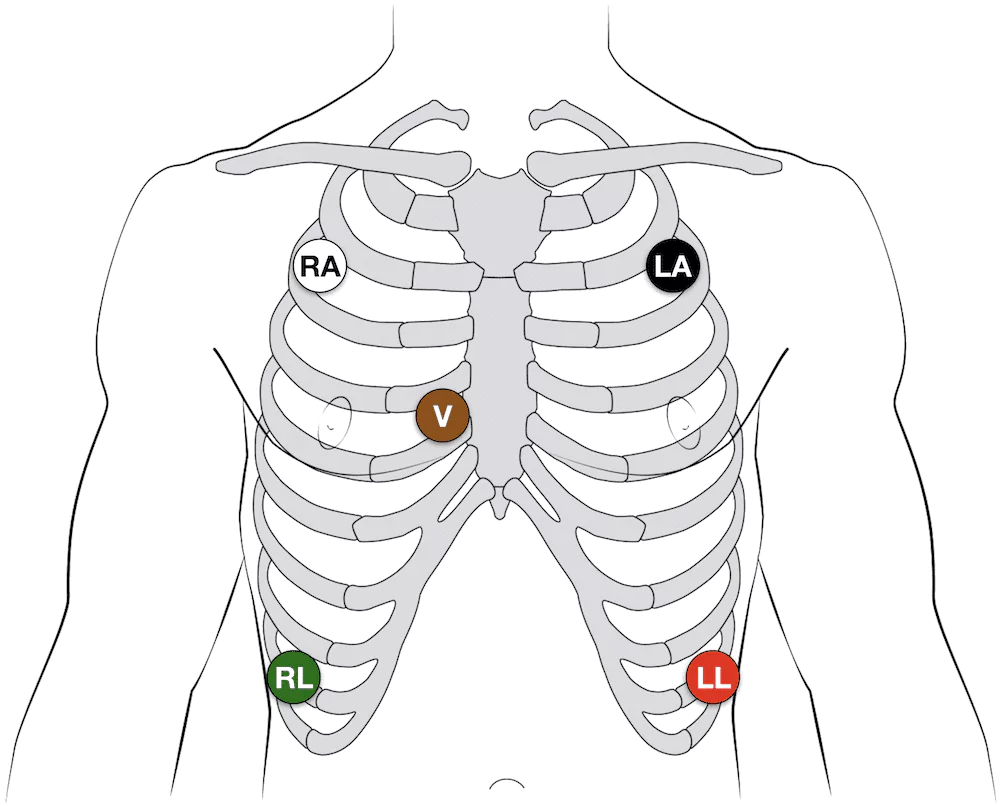
The standard 12-lead ECG uses 10 electrodes to create 12 different electrical “views” of the heart. This isn’t just electrode placement, it’s advanced electrical engineering:
- Limb leads (I, II, III): Form Einthoven’s triangle, measuring potential differences between limbs
- Augmented leads (aVR, aVL, aVF): Created by the machine’s electronics, not direct electrode measurements
- Precordial leads (V1-V6): Measure electrical activity across the chest wall
- Wilson central terminal: A reference point created by averaging the limb lead potentials
The machine’s electronics must continuously calculate these derived leads while maintaining electrical safety and signal integrity.
Common Challenges: What Goes Wrong and Why
The Top 5 ECG Failures (And How to Fix Them)
Based on field experience and service data, here are the failures that cause 80% of ECG downtime:
1. Poor Data Acquisition (35% of failures)
- Symptoms: Weak signals, missing beats, irregular baseline
- Common causes: Electrode placement errors, dried gel, loose connections
- Quick fix: Check electrode impedance using the machine’s built-in test function
- Prevention: Replace electrodes every 24 hours, ensure proper skin prep
2. Noise and Artifacts (25% of failures)
- Symptoms: Wandering baseline, 60Hz interference, muscle artifact
- Common causes: Patient movement, electrical interference, ground loops
- Quick fix: Use proper grounding, check for nearby electrical equipment
- Prevention: Maintain environmental controls, regular cable inspection
3. Power and Battery Issues (20% of failures)
- Symptoms: Unexpected shutdowns, calibration drift, memory loss
- Common causes: Battery age, power supply fluctuations, charging system faults
- Quick fix: Test battery voltage, check power connections
- Prevention: Replace batteries on the manufacturer’s schedule, use UPS systems
4. Cable and Connection Problems (12% of failures)
- Symptoms: Intermittent signals, lead-off alarms, signal dropouts
- Common causes: Cable fatigue, connector corrosion, internal wire breaks
- Quick fix: Wiggle test cables, clean connectors with approved solutions
- Prevention: Proper cable management, avoiding sharp bends, and regular inspection
5. Software and Calibration Issues (8% of failures)
- Symptoms: Incorrect measurements, calibration errors, interpretation failures
- Common causes: Software bugs, calibration drift, incorrect settings
- Quick fix: Restart system, run automatic calibration sequence
- Prevention: Regular software updates, quarterly calibration checks
The Human Factor: Training and Workflow Challenges
Research reveals that training programs improve ECG technician efficiency by 35%, yet many hospitals struggle with adequate training.
Common workflow issues include:
- Electrode misplacement: Results in diagnostic errors in up to 24% of cases
- Inadequate skin preparation: Causes signal artifacts and repeat procedures
- Documentation gaps: Creates compliance issues and billing problems
- Inefficient workflows: Average setup time can be reduced by 3-4 minutes with proper protocols
Maintenance and Calibration: Keeping Your ECG Running
The Reality of ECG Maintenance
Proper maintenance prevents 90% of ECG accuracy issues, yet many facilities rely only on annual service calls. Here’s what really works:
Daily Maintenance (5 minutes):
- Visual inspection of cables and electrodes
- Battery level check
- Calibration signal verification
- Cleaning of contact surfaces
- Documentation of any anomalies
Weekly Maintenance (15 minutes):
- Electrode impedance testing
- Cable continuity checks
- Print mechanism cleaning
- Software/firmware updates, if available
- Review of error logs
Monthly Maintenance (30 minutes):
- Complete calibration verification
- Power supply testing
- Ground system inspection
- Connector deep cleaning
- Performance data analysis
When to Call for Service vs. Handle In-House
Understanding your capabilities saves time and money:
| Handle In-House | Call for Service |
| Basic calibration adjustments | Internal component replacement |
| Electrode and cable replacement | Complex calibration procedures |
| Software configuration changes | Safety circuit testing |
| Routine cleaning and maintenance | Major software problems |
| Simple troubleshooting procedures | Any issue affecting patient safety |
Modern ECG Technology: Separating Hype from Reality
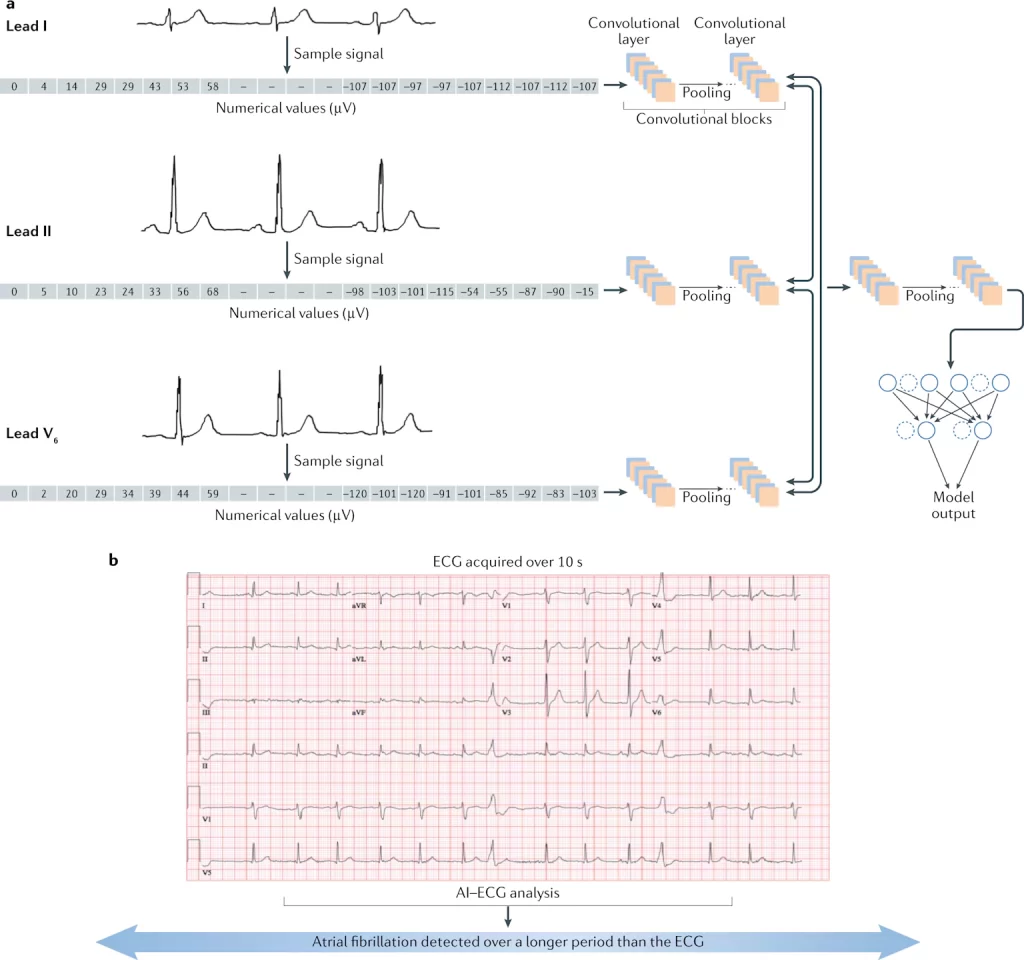
AI-Enhanced ECG: The Real Story
The marketing promises of AI-powered ECG interpretation sound impressive, but the clinical reality is more nuanced. Current AI systems achieve approximately 73% accuracy compared to 85%+ for experienced cardiologists.
This gap becomes critical in emergency situations where false positives or missed diagnoses can have serious consequences.
AI Works Well For:
- Routine screening in low-risk populations
- Quality assurance and second opinions
- Pattern recognition in large datasets
- Workflow efficiency improvements
AI Struggles With:
- Complex arrhythmias require a clinical context
- Artifacts that mimic pathology
- Unusual presentations or rare conditions
- Integration with existing hospital systems
Portable and Telemedicine ECG: Practical Considerations
Portable ECG systems offer flexibility but come with trade-offs that affect clinical decision-making:
| Advantages | Limitations |
| ✔️ Point-of-care testing capabilities ✔️ Reduced patient transport requirements ✔️ Emergency and field medicine applications ✔️ Home monitoring possibilities | ❌ Battery life constraints in field conditions ❌ Signal quality issues in uncontrolled environments ❌ Data transmission and connectivity challenges ❌ Training requirements for non-specialized users |
Cost-Benefit Analysis: The Business Reality
Total Cost of Ownership
When evaluating ECG systems, the purchase price represents only 30-40% of total costs over a typical 7-year lifespan:
Hidden Costs Include:
- Training and certification: $2,000-5,000 per technician
- Maintenance contracts: 8-12% of purchase price annually
- Supplies and consumables: $500-1,200 per year
- Downtime and lost productivity: $12,000+ per hour
- Compliance and documentation: 2-3 hours weekly staff time
ROI Calculations That Matter
Proper ECG management delivers measurable returns:
- 35% improvement in technician efficiency with certification programs
- 90% reduction in equipment failures with preventive maintenance
- 40% decrease in documentation time with optimized workflows
- $2.3M annual savings reported by hospitals implementing comprehensive ECG programs
Practical Takeaways: What You Can Do Tomorrow
For Biomedical Engineers and Technicians:
- Implement daily 5-minute check protocols to catch 80% of potential failures
- Establish quarterly calibration schedules instead of waiting for annual service
- Create troubleshooting flowcharts for your specific equipment models
- Document all maintenance activities for compliance and trend analysis
For ECG Technicians:
- Focus on electrode placement accuracy to reduce diagnostic errors by 20%+
- Develop consistent patient preparation routines to minimize artifacts
- Learn to recognize equipment problems before they affect patient care
- Maintain competency through regular training to improve efficiency by 35%
For Procurement and Management:
- Evaluate the total cost of ownership, not just the purchase price
- Include training costs in budget calculations
- Negotiate comprehensive service contracts that include preventive maintenance
- Plan for technology lifecycle management with 7-year replacement cycles
Conclusion: Beyond the Textbook
Understanding ECG machines isn’t just about knowing how electrodes detect heart signals or how amplifiers work. It’s about recognizing that behind every waveform is a patient whose care depends on your equipment working flawlessly and your team understanding how to use it effectively.
Your expertise in ECG technology doesn’t just keep equipment running; it keeps hearts beating and saves lives. That responsibility deserves both respect and the practical knowledge to handle whatever challenges come your way, whether it’s during routine maintenance or emergency troubleshooting when every second counts.
Remember: in the world of cardiac care, there are no small equipment problems, only equipment problems that haven’t affected patient outcomes yet. Your understanding of ECG machines and commitment to their proper operation stand between technology and the patients who depend on it.
Have questions about ECG Machine technology or want to share your experience? Join the discussion in our biomedical engineering community forum where professionals collaborate and learn from each other’s expertise.